World Heart Rhythm Week 2020 | Understanding Atrial Fibrillation
World Heart Rhythm Week is an annual event is organised by the Arrhythmia Alliance to promote awareness on detecting arrhythmias (irregular heart rhythm). Irregular heart rhythm or known medically as atrial fibrillation (AF or Afib) is the commonest heart rhythm disease in the world, affecting up to 33.5 million people worldwide (according to a study) and is continuing to increase annually. AF is associated with increased risk of strokes, death and heart failure therefore recognising AF is very important. If you want to learn more about AF, please see my previous post (link to previous post).
The message this year is "Don't Miss A Beat" which emphasises the importance of pulse checks, which can decrease the number of sudden cardiac deaths and undiagnosed atrial fibrillation cases each year.
How to support it?
- Spread the word on social media using the #WorldHeartRhythmWeek #WHRW2020
- Encourage people to check their pulses – this can be done by a simple manual palpation which anyone can do in 30 seconds or if you have a device such as an Apple Watch which can diagnose irregular heart rhythm (atrial fibrillation or afib).
As healthcare professionals, when we are seeing patients, taking 30 seconds when performing physical examination to screen for irregular pulse can help identify asymptomatic AF. Also, take the chance to educate our patients on how to check their own pulse.
How to check your pulse?
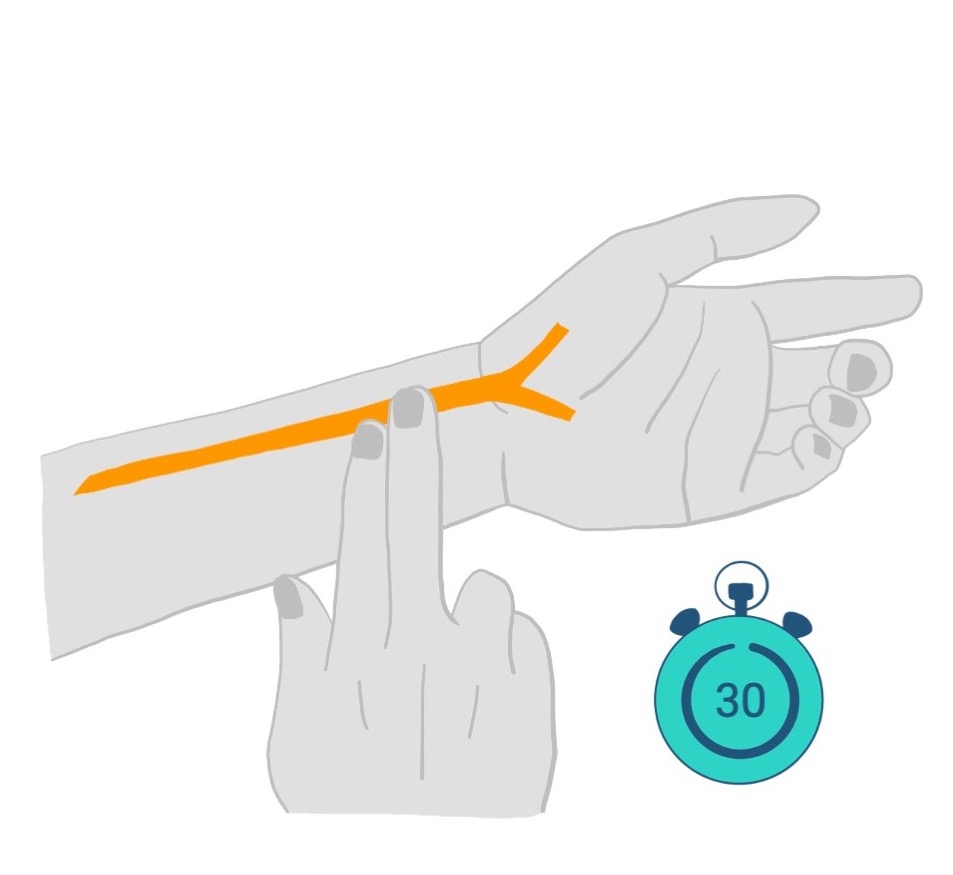
Step 2: Place 3 fingers firmly on along the wrist and you should be able to feel a pulsation just hitting your fingers.
Step 3: Count the number of beats over 30 seconds and multiply that by 2. This will be your heart rate in a minute. Whilst you are counting the heart rate, notice the rhythm – it should be regular i.e. you can predict the next beat. If it is irregular, please contact your healthcare provider as it may be a sign of AF.
You can do this at any time during the day when you get the chance to. This is especially useful when you suffer from symptoms such as palpitations, breathlessness or dizziness and can detect irregularities of your pulse during this period as AF can be transient.
- Not only is the treatment of AF important, addressing the different cardiovascular risk factors linked with AF can reduce the impact of AF on mortality. Ensuring good control of hypertension, encouraging healthy lifestyle habits to promote physical activity and weight loss can all contribute to improving outcomes of our patients.
- Encourage compliance of medications in patients. Educating patients on the rationale behind medications which they are taking and answering questions about them can promote compliance.
Some common medications and the rationale behind their use in AF include:
- Beta-blockers
- Beta-blockers are a class of medications (normally ends with -olol) which slows down the heart rate. It can reduce the symptoms associated with the fast heart rate and is the first choice used to control AF unless there are conditions which does not allow its use. Common side effects lethargy, headache and dizziness.
- Digoxin
- Digoxin is a medication that has previously been commonly used to control heart rate in AF. Its use has subsided with the implementation of betablockers but is still used in some situations. As above, it reduces symptoms by controlling the heart rate. Common side effects include gastrointestinal upset, dizziness, blurred vision and rash.
- Flecainide
- Flecainide is commonly used as a pill-in-the-pocket for patients with AF that occurs infrequently or as a regular tablet to prevent recurrence of AF. Common side effects include dizziness and headaches. The use of flecainide should only be under the instructions of your healthcare practitioner as it requires regular monitoring to ensure its safe use.
- Amiodarone
- Amiodarone is a tablet that is commonly used to restore sinus rhythm in patients with AF. It has to be used in caution as there is an increased risk of other heart rhythm problems when used with certain drugs. Common side effects include nausea, skin discolouration and thyroid issues. The use of amiodarone should only be under the instructions of your healthcare practitioner as it requires regular monitoring to ensure its safety in long-term use.
- ACE inhibitors or ARBs
- Angiotensin Converting Enzyme-inhibitors (normally ends with -pril) or angiotensin receptor blockers (normally ends with -artan) are medications not directly used in the treatment of AF but used to control high blood pressure and improve life expectancy in heart failure, both conditions commonly linked with AF. Common side effects of ACE-inhibitors are dry cough, headache, dizziness and rash whilst ARBs are dizziness, headaches and flu-like symptoms
- Anticoagulation
- As AF is associated with an increased risk of stroke, some patients will need to be protected against this risk with the use of anticoagulation. Warfarin or the newer oral anticoagulants (Rivaroxaban, Apixaban, Dabigatran or Edoxaban) are commonly used in the UK. They work by thinning the blood and reduce the clot forming in the heart chambers that could cause a stroke. The main risk these medications carry is the risk of bleeding. Therefore, one needs to stay vigilant in recognising any bleeding as they may require medical attention.
Summary
It is important to recognise AF as it remains a highly treatable disease with potentially disastrous outcome if left untreated. With the use of technology, we have come a long way to be able to diagnose AF and hopefully this will become more commonplace so we can identify and treat this disease promptly and effectively. For now, the action of palpating the pulse which has been performed throughout the history of medicine will hold the key to identifying more cases and prevent the next stroke! So spread the knowledge!
This post contains affiliate links. For more information please visit my disclaimer page.